It can last 10 years and has significant physical, emotional and mental health repercussions. So why do we know so little about perimenopause? Kate Bussmann meets author and health expert Maisie Hill, who is on a mission to give women the knowledge to help themselves.
Quick quiz: how long does menopause last? Does hormone replacement therapy (HRT) cause cancer? What’s testosterone got to do with menopause? How likely are you to encounter a GP who’s had any training at all in menopause management?
Chances are, if you’re over 40, you might know the answers to some of these questions – or have at least attempted to find them.
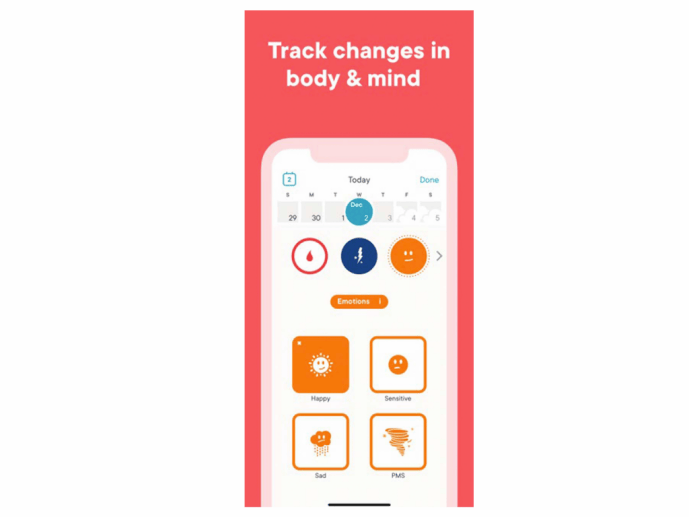
And here’s another, more personal one: do you know the average length of your cycle (if you still have periods)? Perhaps you’re one of the more than 100 million women who use a cycle-tracking app. Maybe you started when you were trying to conceive. Or perhaps, like me and many other 40-somethings, you started using one to work out whether you’re in perimenopause – that is, the typically 10 years during which a woman’s hormone levels shift before she stops having periods, resulting in myriad changes, from irritability and even rage, to sleep issues and hot flushes.
Like me, you might not be willing to wait until things get really bad before you seek help. You might want to know now whether the headaches, mood swings, mental fug, insomnia or extra weight could be related to your hormones – and thus, whether there’s something you can do about them.

Maisie Hill wants to help you with the answers. A women’s health expert who trained in Chinese medicine and worked as a birth doula before writing the 2019 book Period Power, she has now released a sequel, Perimenopause Power, designed to educate and equip women entering this phase of their life. It’s a very big, very readable book – more than 300 pages of information and advice (anchored in a hefty appendix of scientific citations), some of which will make you gasp at how ill-informed you are about your own body.
A mother of one, Maisie is only 40 – this didn’t begin as a first-person story. “Selfishly, I wanted to do the research for myself ahead of time,” she admits. “But women are so thirsty for this information. I know I do a good job of explaining things, particularly making scientific literature accessible, so I didn’t want to wait 10 years. This is a phase of life in which support is needed,” she explains.
Before you start thinking that your GP is busy enough right now, consider this: women in midlife are linchpins in society, likely to be burdened with the lion’s share of childcare and housework, as well as attempting to hold down a job and care for parents. And if you’re dealing with all that when your health and overall wellness are below par, and there are interventions that will help, you don’t just deserve them, you need them.
“It’s a perfect storm, and when you add hormonal shifts and the challenges of recent lockdowns, there’s a lot to overcome to actually get to the GP and ask questions,” says Maisie. “We’re socialised to accept that menstrual and perimenopausal symptoms are just part of having a female reproductive system – that’s something we have to get over. We need to share more and require more and get better access to care.”
So, to those questions. Menopause does not refer to the years when your cycle goes haywire or the years after your period stops. It is a single day: the one-year anniversary of your last ever period, and happens on average at the age of 50 or 51.
Postmenopause is the third of your life that follows and perimenopause is the decade or so leading up to it. But oestrogen doesn’t simply gradually fade away, taking with it your periods. In fact, they may initially get more frequent, owing in part to a reduction in the progesterone that regulates the second half of your cycle. Maisie describes this stage as “very early menopause” (not to be confused with “early” or “premature” menopause, when periods stop before the age of 40). This then segues into “early perimenopause”. It’s in “late perimenopause” that your cycle may lengthen, as oestrogen falls.
This is why Maisie is a strong advocate of cycletracking. “The data you collect can be helpful to you, but also to take to a healthcare professional and say, ‘These are my symptoms, this is how long it lasts for, and this is how it’s been evolving.’” That information is far more helpful than the blood tests doctors often order to check hormone levels. “For women aged 45 and up, blood tests in themselves aren’t actually a reliable way of determining whether someone is perimenopausal because hormones are released in pulses and vary from cycle to cycle.
“The current recommendations aren’t that someone has to have particular blood test results in order to be told they’re perimenopausal.” Instead, the UK’s National Institute for Health and Care Excellence and the Australasian Menopause Society guidelines say perimenopause should be diagnosed based on vasomotor symptoms (hot flashes, sweating and heart palpitations) and irregular periods.
“Which is why it’s so important to go to your GP with an awareness of what’s going on with your cycle. If someone was to have HRT, that will point to what specific formulations would work well. Ideally, it’s an ongoing conversation – as hormone levels change and you maybe go from having plenty of oestrogen to not much oestrogen, then your prescription will shift.”
It also helps simply to understand what’s happening, which is why those delineated phases of perimenopause can be a light-bulb moment. “I think it’s helpful when we can name something, and say, ‘Maybe you’re in this phase, these are the common things that can happen, and this is what’s going on.’”
If your doctor suggests HRT, the question of whether or not to take it can be a fraught one, whether from a notion that menopause is a natural process that should run its course or concerns over the safety of HRT.
In her book, Maisie unpicks exactly how those ideas became mainstream. In 2002, early data from a study by the Women’s Health Initiative was sent to UK journalists. The resulting headlines were terrifying: that HRT causes a 26% increase in breast cancer, a 29% increase in heart attacks, and a 41% increase in stroke among women using a particular pair of HRT drugs.
Unsurprisingly, prescription rates plummeted, but when the data was released, it was far less alarming. The increase in breast cancer was not proven to be statistically significant.
What’s more, under scrutiny, the study itself proved unreliable. Increased risk of stroke or heart attack was only seen in the women who had been postmenopausal for 20 or more years; 70% of them were very overweight or obese.
“There were participants who already had significant health issues, so there’s a problem with the actual data that was collected,” notes Maisie. “The analysis of that data was flawed. Also, the forms of HRT used are outdated.”
In fact, a 2006 meta-analysis of multiple studies showed HRT reduced coronary heart disease in younger women (but not older).
As for just letting nature take its course? “Menopause can be both a positive transition and a situation where the use of hormones, along with other lifestyle measures, can be hugely helpful.
It’s a stage of life, not a disease. For some reason, our hormones are meant to decline in midlife, which is why I’m not a fan of the term hormone replacement therapy, because it implies we should have hormones.” She prefers the more neutral “menopausal hormone therapy” or MHT.
The subject of language and what it’s freighted with comes up repeatedly in her book. The word “hysterectomy” comes from “hysteria”, and all that implies; vets use “uterectomy” instead.
Maisie uses the term “genito-urinary syndrome of menopause” (GSM) to describe the effects of less oestrogen on your vulva, vagina and lower urinary tract that include painful sex and UTIs. Better that than the kegel-clenchingly horrible term “vulvovaginal atrophy”.
Terminology, she argues, really does matter, especially with embarrassing symptoms: only 25% of women with GSM, she says, will go to a healthcare practitioner about it.
Perception matters too, as in the case of testosterone, which is made in your ovaries and adrenal glands; it is not a male hormone. “Production decreases after menopause,” she says, and low levels can cause “mood swings, belly fat, low energy, brain fog, low sexual desire, low muscle mass and bone loss”.
But in many places, including New Zealand, testosterone is not licensed to help women’s sexual desire, mood or concentration, and so has to be prescribed “off-label”, if at all.
As for the last question: according to a 2017 survey by menopause specialist Dr Louise Newson only 52% of UK GPs had any training in menopause management, a fact that saddens Maisie.
“Some people have a very positive experience of perimenopause and menopause, but some lose their self-confidence and identity. There can be really rapid changes – and if you have no idea why, that’s going to cause damage. The early fifties is when women are at greatest risk of suicide. Is it coincidental that that’s when oestrogen drops off, and you get cognitive and mood changes?
There can be really rapid changes – and if you have no idea why, that’s going to cause damage
“With pregnancy, there are all these specialists – it’s a whole field of medicine,” she adds. “But we’ve got the childbirth year and the perimenopause decade, and we spend a third of our lives as postmenopausal women. We need more, and we need it better.”
Your Perimenopause Toolkit
Resistance training
“Now is the time to start resistance training,” says Maisie. Weight-bearing and strength exercises in your perimenopausal years help build bone density and bone resilience.
Vitamin B
Vitamin B6 can support progesterone production, reduce inflammation and improve PMS and other mood-related issues.
Cycle-tracking
Clue, a cycle-tracking app that lets you input everything including physical and emotional symptoms.
Lubricant
“I’m a fan of lube at any age – it makes such a difference to our experience of pleasure,” says Maisie.
Multi duvet
Suffering night sweats? If you share a bed, Maisie recommends the Scandi way: buy two single duvets instead of a large one so you can regulate your own temperature. Moisture-wicking wool-filled duvets can also help.
Words via Kate Bussmann / Stella magazine.